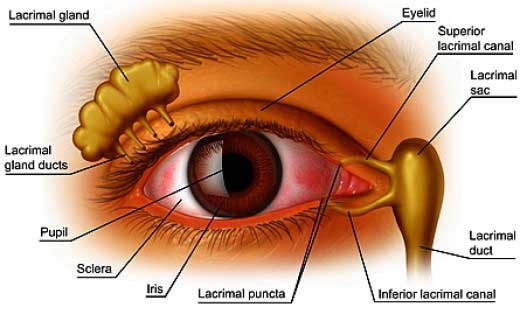
 The ocular tear film is a surprisingly complex mix of 3 main constituents; a water layer produced by the lacrimal gland, mucous produced by the surface cells of the conjunctival epithelium (surface ‘skin’ layer) of the eye and a oily lipid component from the meibomium glands of the eyelid margin. Any deficiency or imbalance in these components will create an instability of the tear film which can result in an incomplete coating of the ocular surface. A poor tear film in either quality or quantity combined with rapid elimination of tears from the ocular surface due to tear film drainage or evaporation will cause a dry eye situation. In general terms, 30% of tears are lost from the ocular surface by drainage through the upper and lower lid tear drainage ducts and 70% by evaporation.
The ocular tear film is a surprisingly complex mix of 3 main constituents; a water layer produced by the lacrimal gland, mucous produced by the surface cells of the conjunctival epithelium (surface ‘skin’ layer) of the eye and a oily lipid component from the meibomium glands of the eyelid margin. Any deficiency or imbalance in these components will create an instability of the tear film which can result in an incomplete coating of the ocular surface. A poor tear film in either quality or quantity combined with rapid elimination of tears from the ocular surface due to tear film drainage or evaporation will cause a dry eye situation. In general terms, 30% of tears are lost from the ocular surface by drainage through the upper and lower lid tear drainage ducts and 70% by evaporation.
The common symptoms associated with ocular dryness include redness, grittiness, burning, ocular fatigue and ache, light sensitivity (photophobia) and sometimes reflex (paradoxical) tearing. The severity of symptoms experienced will be dependent upon several inter-related factors. These include the quantity of tear being produced; environmental factors, in particular the ambient humidity and air flow over the ocular surface; any associated medical conditions that may impact on the way the tears are distributed over the ocular surface. Consequently a patients symptoms may vary from day to day and in different situations.
Local ocular surface disease such as chronic blepharitis with associated inflammation of the meibomium gland of the eyelids will usually cause the oil product of the glands to be of poor quality. This in turn will cause the water component of the tears to evaporate rapidly. Similarly, loss of conjunctival mucous producing cells may cause the oil and water components of the tears to bind poorly to the conjunctival and corneal cells thus incompletely moisturizing the surface of the eye. Certain scaring diseases of the ocular surface may also cause damage or obstruction to the small ducts that allow the water component to be released on the ocular surface, reducing the tear film water volume.
There are a few important medical conditions that maybe associated with dry eyes. Certain auto-immune connective tissue diseases (in particular rheumatoid arthritis, Sjogren’s Disease) and sarcoidosis may cause damage to the lacrimal glands thereby reducing tear film water volume. Thyroid gland under or over activity may also affect the tear film presumably by affecting the mucous layer in a complex mechanism.
Management of dry eye requires treating any localized ocular surface disorder such as blepharitis; acknowledging the role any systemic diseases may play in exacerbating the disease process; managing environmental and lifestyle factors that may impact, such as low humidity (using a room humidifier or limiting use of air conditioners) and increasing blink rates whilst watching television, reading or driving; using ocular lubricants regularly; occasionally conserving tear film volume by inserting punctual plugs that reduce tear film drainage. Usually treatment amounts to regular administration of ocular lubricant drops by day and sometimes thicker gels or ointments at night, treating ocular surface inflammatory disease with appropriate medication, reducing tear film evaporation and drainage as much as possible. With intensive and active treatment it will still usually take 4 to 8 weeks before the ocular surface heals satisfactorily and symptoms reduce or come under control.
For further information and advice, please contact your Ophthalmologist.
For further information regarding this treatment contact our Clinic for expert advice from one of our specially trained Doctors
Patients who are suitable for SLT are glaucoma patients who have not responded effectively to medical treatment, glaucoma patients who are unable to tolerate medical (drop) treatment due to side effects and patients who have had previous ALT treatment.
The treatment is undertaken using topical anaesthetic through a laser contact lens. It takes approximately 10 minutes for an eye to be treated with patients able to leave the clinic immediately following treatment without pain or significant blurring of vision. The treated eye may be sensitive to light for 12 to 24 hours post treatment, and patients will need to return for review 1 to 2 weeks and again 4 to 8 weeks after treatment to check the IOP. Patients who undergo SLT treatment should expect IOP to drop within 1 to 3 weeks following treatment.
Further information regarding SLT can be obtained from www.ellex.com.au or please contact the staff at Waverley Eye Clinic.
